Radiotherapy Simulation
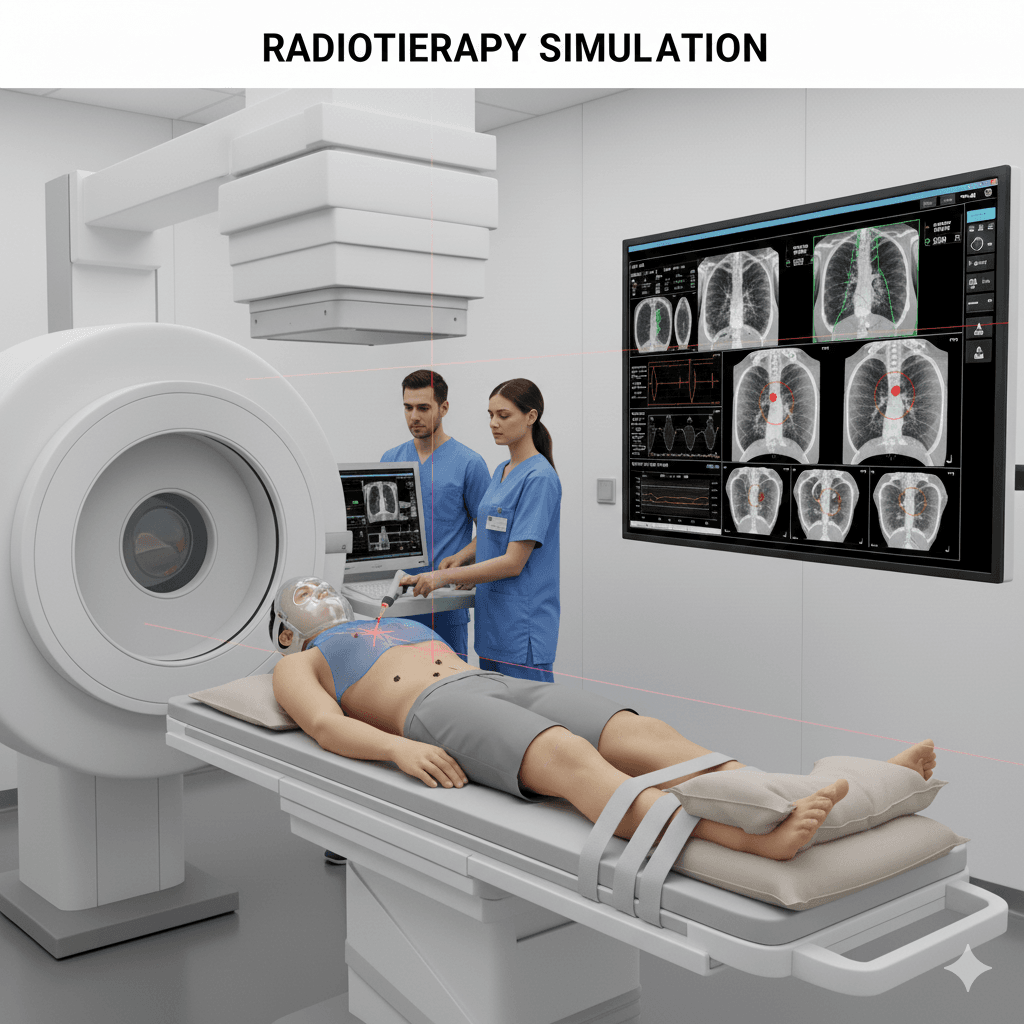
Q1: What is CT or MRI simulation in radiotherapy treatment?
A: CT (Computed Tomography) or MRI (Magnetic Resonance Imaging) simulation is a crucial step in the planning process for radiotherapy treatment. These imaging techniques are used to create detailed, three-dimensional pictures of the area to be treated. This allows the radiation oncology team to precisely target the tumor while sparing surrounding healthy tissues.
Q2: Why is imaging simulation important in radiotherapy?
A: Imaging simulation is important because:
- Precise targeting: It helps accurately locate the tumor and define its shape, size, and position relative to nearby organs and tissues.
- Customized treatment: The detailed images enable the creation of a personalized treatment plan that delivers the optimal radiation dose to the tumor while minimizing exposure to healthy tissues.
- Improved outcomes: Accurate imaging improves the effectiveness of radiotherapy and reduces the risk of side effects.
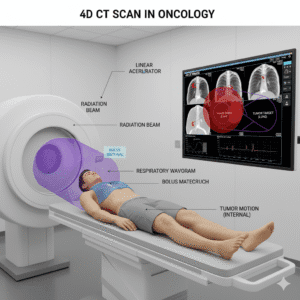
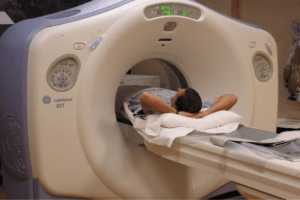
Q3: How is a CT simulation performed?
A: A CT simulation involves the following steps:
- Positioning: You will lie on a CT scanner table in the same position you will be in during your radiotherapy treatments. Immobilization devices may be used to help you stay still.
- Imaging: The CT scanner takes a series of detailed X-ray images from different angles, which are then combined to create a 3D picture of the treatment area.
- Marking: Temporary or permanent marks may be placed on your skin to help align the radiation beams accurately during each treatment session.
- Planning: The images are used by the radiation oncologist and dosimetrist to design a treatment plan that targets the tumor precisely.
Q4: How is an MRI simulation performed?
A: An MRI simulation involves the following steps:
- Positioning: Similar to CT simulation, you will lie on an MRI scanner table, and immobilization devices may be used to ensure you stay in the correct position.
- Imaging: The MRI scanner uses powerful magnets and radio waves to produce detailed images of the treatment area. The process is non-invasive and does not use ionizing radiation.
- Contrast agents: In some cases, a contrast agent may be injected to enhance the images and provide more detailed information about the tumor and surrounding tissues.
- Planning: The images are used by the radiation oncology team to develop a precise treatment plan.
Q5: What are the differences between CT and MRI simulations?
A: The key differences between CT and MRI simulations include:
- Imaging technology: CT uses X-rays to create images, while MRI uses magnetic fields and radio waves.
- Image detail: MRI provides superior soft tissue contrast and can better differentiate between different types of tissues, making it ideal for imaging the brain, spinal cord, and other soft tissues. CT is better for imaging bones and is faster.
- Radiation: CT involves exposure to a small amount of ionizing radiation, whereas MRI does not use radiation.
The choice between CT and MRI simulation depends on the specific clinical situation and the area being treated.
Q6: What should I expect during the simulation process?
A: During the simulation process:
- Comfort: You will be positioned on a table, and it’s important to stay as still as possible to ensure accurate images. The positioning may take some time, but the healthcare team will ensure you are as comfortable as possible.
- Noise: MRI machines can be noisy, so you may be given earplugs or headphones. CT scans are quieter and faster.
- Duration: A CT simulation typically takes about 10-30 minutes, while an MRI simulation may take 30-60 minutes, depending on the complexity of the images needed.
- Communication: The technologist will be in constant communication with you to guide you through the process and address any concerns.
Q7: Are there any risks or side effects associated with CT or MRI simulation?
A: Both CT and MRI simulations are generally safe procedures:
- CT risks: The primary risk is exposure to a small amount of ionizing radiation. However, the benefits of accurate tumor targeting typically outweigh this risk.
- MRI risks: There are no known risks from the magnetic fields and radio waves used in MRI. However, patients with certain implants, such as pacemakers, may not be able to undergo an MRI. Additionally, some people may experience discomfort or allergic reactions to the contrast agent used in MRI.
Your Clinical (Radiation) Oncologist will discuss any potential risks with you before the procedure.
Q8: How do I prepare for a CT or MRI simulation?
A: Preparation for a CT or MRI simulation may include:
- Clothing: Wear comfortable, loose-fitting clothing. You may be asked to change into a gown.
- Metal objects: Remove any metal objects, such as jewelry, glasses, and hairpins, as they can interfere with imaging, particularly for MRI.
- Diet: Follow any specific instructions regarding eating or drinking, especially if a contrast agent will be used.
- Medical history: Inform your healthcare team of any medical conditions, allergies, or implants you may have.
If you have more questions about CT or MRI simulation or need additional information on how these imaging techniques will be used in your radiotherapy treatment, you may book an appointment with Dr Ruchir Bhandari. You will be provided with detailed information and he will guide you through the preparation and procedure to ensure the best possible outcome.
Related Post

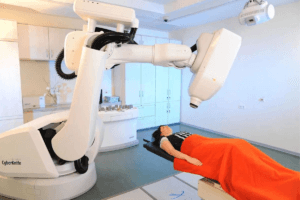
CyberKnife
August 6, 2024

Immunotherapy
August 7, 2024

MRI Linac
August 7, 2024
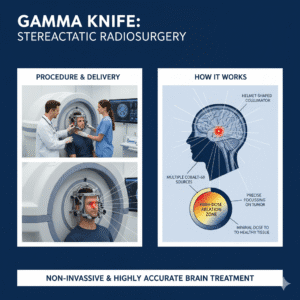
Gamma Knife
August 7, 2024
Cancer Screening
August 22, 2024
Gallery
Click below to book a clinic appointment
Ask More Questions Send Query On Email