Cancer Info
Breast Cancer
What are the risk factors for breast cancer?
Breast cancer risk factors include a mix of genetic, lifestyle, and environmental influences. Being female is the most significant risk factor, as women are much more likely to develop breast cancer than men. Age is another crucial factor; the risk increases as women get older, especially after age 55. Family history plays a significant role; if you have close relatives with breast cancer, your risk is higher. Genetic mutations, particularly in the BRCA1 and BRCA2 genes, can dramatically increase risk. Lifestyle factors, such as being overweight, not getting enough physical activity, and consuming alcohol excessively, also contribute to the likelihood of developing breast cancer.
How can I get screened for breast cancer?
Screening for breast cancer primarily involves mammograms, which are specialized X-ray images that can detect tumors before they can be felt. Women are generally advised to begin regular mammogram screenings at age 40, but those with a family history or other risk factors may need to start earlier. Clinical breast exams, conducted by a healthcare provider, involve a physical examination of the breasts and can help identify any changes. Additionally, self-exams at home can help women become familiar with their breasts and notice any unusual lumps or changes.
What tests are done to diagnose breast cancer?
Diagnosis begins with imaging tests. A mammogram may reveal abnormalities, prompting further investigation. If something suspicious is found, an ultrasound may be performed to provide more detailed images. The definitive test for diagnosing breast cancer is a biopsy, where a small sample of tissue is removed from the breast. This sample is then examined under a microscope to check for cancer cells. There are different types of biopsies, such as fine-needle aspiration or core needle biopsy, depending on the situation.
What role does chemotherapy play in treatment?
Chemotherapy is a systemic treatment that uses powerful drugs to target and kill cancer cells throughout the body. It is often recommended after surgery (adjuvant chemotherapy) to eliminate any remaining cancer cells and reduce the risk of recurrence. In some cases, chemotherapy is given before surgery (neoadjuvant chemotherapy) to shrink large tumors, making them easier to remove. The specific chemotherapy regimen varies depending on the type of breast cancer, its stage, and individual patient factors, and it may involve a combination of drugs.
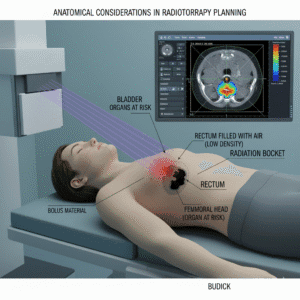
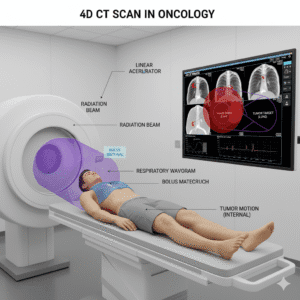
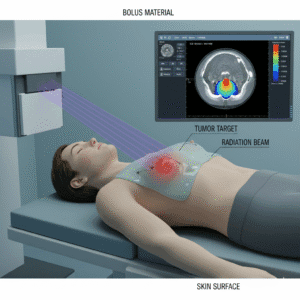
How does radiotherapy work?
Radiotherapy, or radiation therapy, uses high-energy radiation (like X-rays) to destroy cancer cells. It is particularly effective at targeting localized tumors and is commonly used after breast-conserving surgery (lumpectomy) to reduce the risk of the cancer coming back in the same area. The treatment is usually delivered over several sessions, often five days a week for several weeks. Side effects may include skin irritation, fatigue, and changes in breast sensation, but these are typically manageable and temporary.
Will I need surgery?
Surgery is a central component of breast cancer treatment for many patients. The type of surgery recommended depends on the size, location, and stage of the cancer. A lumpectomy involves removing the tumor and a small margin of surrounding tissue, while a mastectomy involves removing one or both breasts. In some cases, nearby lymph nodes may also be removed to check for cancer spread. The decision about the type of surgery takes into account the patient’s preferences, overall health, and specific cancer characteristics.
What can I expect during follow-up appointments?
Follow-up appointments are essential for monitoring recovery and ensuring there are no signs of cancer recurrence. During these visits, your healthcare provider will conduct a physical exam, review any new symptoms or concerns, and may order imaging tests like mammograms or ultrasounds as needed. The frequency of these follow-ups often decreases over time but may be more frequent in the first few years after treatment.
Are there genetic factors involved in breast cancer?
Genetics play a significant role in breast cancer risk. Certain inherited genetic mutations, especially in the BRCA1 and BRCA2 genes, can greatly increase a person’s risk of developing breast cancer, sometimes as high as 70% by age 80. Genetic counseling is recommended for individuals with a family history of breast or ovarian cancer, as it can help assess risk, discuss genetic testing options, and consider preventive measures.
What rehabilitation services are available?
Rehabilitation services can play a vital role in recovery. Physical therapy can help regain strength and mobility, especially after surgery. Speech therapy may be needed for some patients if they experience changes in speaking or swallowing. Emotional support through counseling or support groups is also crucial for addressing mental health challenges. Occupational therapy can assist patients in adapting to any physical limitations in daily activities.
What should I eat during treatment?
Nutrition is a key part of supporting health during breast cancer treatment. A well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins is essential for providing the necessary nutrients and energy. Staying hydrated is also crucial, especially if side effects like nausea or dry mouth occur. Nutritional needs can vary based on treatment side effects, so discussing specific dietary recommendations with a healthcare provider or nutritionist is beneficial.
While no specific foods cause or cure breast cancer, certain dietary choices can support overall health and recovery. It’s advisable to limit processed foods, excessive sugar, and high-fat foods, as well as to minimize alcohol intake, which can negatively impact treatment outcomes. Some patients may need to avoid spicy, acidic, or crunchy foods if they experience mouth sores or other treatment-related side effects.
How does stress affect my cancer treatment?
Stress can have a significant impact on overall health and well-being, potentially influencing how well the body responds to cancer treatment. High levels of stress may weaken the immune system and contribute to feelings of anxiety and depression. Finding effective stress management techniques, such as mindfulness, meditation, yoga, or joining support groups, can help improve emotional health and enhance coping during treatment.
How important is exercise during treatment?
Exercise is highly beneficial during and after breast cancer treatment. Engaging in physical activity can help reduce treatment-related fatigue, improve mood, and enhance overall physical function. Regular exercise, such as walking, swimming, or yoga, can be adapted to individual energy levels and health status. It’s essential to consult your healthcare team before starting any new exercise regimen to ensure it’s safe and appropriate.
What are my options for breast reconstruction?
Breast reconstruction is an option for women who have had a mastectomy. There are two main types of reconstruction: implant-based reconstruction and autologous reconstruction, where tissue is taken from another part of the body (like the abdomen) to create a new breast. The timing of reconstruction can be immediate (during the same surgery as the mastectomy) or delayed (at a later date). Each option has its benefits and considerations, so discussing them with a surgeon who specializes in breast reconstruction is important.
What resources are available for support?
Many resources are available to support patients through their breast cancer journey. Hospitals often offer support groups where patients can connect with others facing similar challenges. Organizations like the American Cancer Society provide educational materials, counseling services, and online resources. Additionally, local community organizations may offer workshops, exercise programs, and financial assistance, helping patients navigate their diagnosis and treatment.