Cancer Info
Cervical cancer
How common is cervical cancer in India?
Cervical cancer is one of the leading cancers among women in India. According to recent statistics, it is the second most common cancer in Indian women, following breast cancer. The incidence is particularly high in rural areas due to limited access to healthcare services, awareness, and screening programs. Increased awareness and vaccination efforts are crucial to reducing this incidence.
What are the risk factors for cervical cancer?
Several risk factors can increase the likelihood of developing cervical cancer:
Human Papillomavirus (HPV) Infection: The primary cause of cervical cancer. Certain high-risk HPV types, particularly HPV-16 and HPV-18, are linked to most cases.
Early Sexual Activity: Beginning sexual activity at a young age increases exposure to HPV.
Multiple Sexual Partners: Having many sexual partners or a partner with a history of multiple partners can increase risk.
Immunosuppression: Conditions that weaken the immune system, such as HIV/AIDS, can make it harder for the body to clear HPV infections.
Smoking: Tobacco use can increase the risk of cervical cancer.
Long-term Use of Oral Contraceptives: Prolonged use may slightly increase risk, though this effect diminishes after stopping the pill.
How is cervical cancer screened for?
Screening for cervical cancer usually involves two tests:
Pap Smear: This test checks for precancerous changes in cervical cells. Women should start getting Pap smears at age 21 and continue every three years until age 29. From ages 30 to 65, they may opt for a Pap smear every three years or a combination of Pap and HPV testing every five years.
HPV Testing: This test detects the presence of high-risk HPV types. It is often done alongside the Pap smear for women over 30.
What are the signs and symptoms of cervical cancer?
In its early stages, cervical cancer may not cause any symptoms. However, as it progresses, symptoms can include:
Abnormal Vaginal Bleeding: This may occur between periods, after intercourse, or after menopause.
Unusual Vaginal Discharge: Changes in discharge, such as increased volume, or discharge with a foul odor.
Pelvic Pain: Persistent pain in the pelvic area not related to menstrual cramps.
Pain during Intercourse: Discomfort or pain during sexual activity.
Can cancer spread to other parts of the body?
Yes, cancer can spread to other parts of the body through a process called metastasis. When cancer cells break away from the original tumor, they can travel through the bloodstream or lymphatic system to other areas of the body, forming new tumors.
What is the role of the HPV virus and vaccination in cervical cancer prevention?
The HPV virus is the leading cause of cervical cancer. Vaccination against HPV can significantly reduce the risk of cervical cancer. In India, the HPV vaccine is recommended for girls aged 9 to 14, ideally before they become sexually active. Two doses of the vaccine are administered six months apart. The vaccine is effective against the most common high-risk HPV types that cause cervical cancer.
How do smoking and alcohol affect the risk of cervical cancer?
Smoking is a known risk factor for cervical cancer, as it can weaken the immune system and make it harder for the body to clear HPV infections. Women who smoke are more likely to develop cervical cancer than non-smokers. Alcohol consumption may also increase the risk, especially when combined with smoking. Quitting smoking and moderating alcohol intake are essential for reducing risk.
What investigations are done to diagnose cervical cancer?
Diagnosis typically involves:
Pelvic Examination: A thorough examination of the reproductive organs.
Pap Smear and HPV Testing: To detect any abnormal cells or high-risk HPV.
Colposcopy: If abnormalities are found, a colposcopy is performed to examine the cervix more closely, using a magnifying instrument. A biopsy may be taken for further analysis.
Imaging Tests: CT scans, MRIs, or PET scans may be used to determine the extent of cancer and whether it has spread.
What is stage-wise management for cervical cancer?
Management of cervical cancer is based on its stage:
Stage 0: Carcinoma in situ is treated with excisional procedures like LEEP or conization.
Stage I: Early-stage invasive cancer often requires surgery, such as a radical hysterectomy, possibly combined with radiation.
Stage II: Surgery is typically followed by radiation and chemotherapy.
Stage III: Treatment usually involves radiation and chemotherapy, as surgery may not be an option.
Stage IV: Advanced cancer may be managed with chemotherapy, palliative care, or clinical trials.
What are molecular tests, and why are they important?
Molecular tests analyze cancer cells for specific genetic changes that may influence treatment decisions. For cervical cancer, tests can identify HPV types and mutations that could predict responses to certain therapies. This information helps in tailoring personalized treatment plans, improving effectiveness, and minimizing side effects.
What role does chemotherapy play in treating cervical cancer?
Chemotherapy is used for more advanced cervical cancer or when there’s a high risk of recurrence after surgery. It involves using drugs that kill rapidly dividing cells, including cancer cells. Common regimens may include combinations of cisplatin, carboplatin, and paclitaxel. Side effects can include nausea, fatigue, hair loss, and an increased risk of infections.
How does immunotherapy work for cervical cancer?
Immunotherapy helps the immune system recognize and attack cancer cells. For cervical cancer, treatments like immune checkpoint inhibitors (e.g., pembrolizumab) are used, particularly for advanced stages. These drugs help remove the “brakes” on the immune system, allowing it to better target and destroy cancer cells.
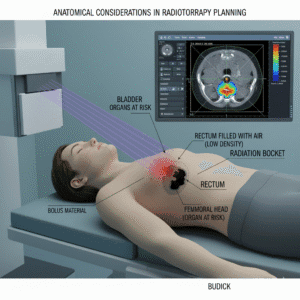
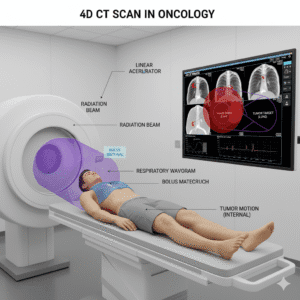
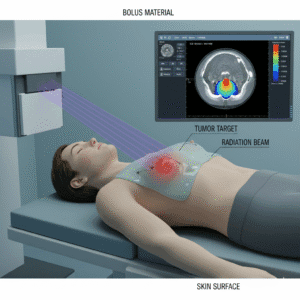
What is the role of radiotherapy in treating cervical cancer?
Radiotherapy uses high-energy rays to kill cancer cells. It can be used:
As a Primary Treatment: For early-stage cervical cancer, often combined with surgery.
After Surgery: To eliminate remaining cancer cells and reduce recurrence risk.
For Advanced Cancer: To control symptoms and reduce tumor size. Side effects may include fatigue, skin irritation, and urinary changes.
What is CyberKnife radiosurgery, and what are its benefits?
CyberKnife is a non-invasive form of stereotactic radiosurgery that delivers precise radiation to tumors. Benefits include:
Non-Invasive: No surgical incisions are required.
Precision Targeting: Real-time imaging allows for accurate targeting of tumors while sparing healthy tissue.
Short Treatment Course: Typically completed in a few sessions.
Minimal Side Effects: Fewer side effects compared to conventional radiation therapy.
What can I expect during follow-up appointments?
Follow-up appointments are crucial for monitoring recovery and detecting recurrence. These visits often involve:
Physical Examinations: Checking for any signs of cancer recurrence.
Pap Smears and HPV Testing: To monitor cervical health.
Imaging Studies: As needed, based on individual circumstances.
Follow-up schedules typically become less frequent over time but remain important for several years post-treatment.
How can exercise help in rehabilitation after cancer treatment is over?
Exercise: Regular physical activity can enhance overall health, support recovery, and help manage treatment side effects. It’s advisable to engage in safe, moderate exercise during recovery.
Rehabilitation: Rehabilitation may include physical therapy and counseling to support recovery, particularly if surgery affects mobility or function.
What diet is recommended?
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support recovery. Consulting with a nutritionist can help tailor dietary recommendations to individual needs.
How will cancer treatment affect my sexual function and fertility?
Cervical cancer treatments can impact sexual function and fertility. It’s important to discuss these concerns with your healthcare provider to explore options, including assisted reproductive technologies.
Can I become pregnant after the treatment is over?
Women with a history of cervical cancer can often have successful pregnancies, but it’s essential to discuss family planning with a healthcare team to understand any risks and considerations.