Cancer Info
Lung Cancer
What are the risk factors for lung cancer?
The primary risk factor for lung cancer is smoking, which is responsible for about 85% of cases. Exposure to secondhand smoke can also increase risk. Other significant risk factors include exposure to radon gas, asbestos, and other carcinogens found in certain workplaces. Additionally, a family history of lung cancer and having certain lung diseases (like COPD) can elevate risk. Age is another factor, as lung cancer is more common in older adults.
How is lung cancer screened for, and what is low-dose CT?
Screening for lung cancer is typically done using low-dose computed tomography (CT) scans. This type of scan uses less radiation than standard CT scans and can detect lung cancer at an earlier stage, which may improve outcomes. The U.S. Preventive Services Task Force recommends annual screening for high-risk individuals, such as those aged 50 to 80 with a history of heavy smoking (e.g., a 20 pack-year smoking history).
How do smoking and alcohol affect lung cancer risk?
Smoking is the most significant risk factor for lung cancer, significantly increasing the likelihood of developing the disease. The risk is even higher for those who smoke heavily or start at a young age. While alcohol consumption is more closely associated with cancers of the head and neck, esophagus, and liver, heavy alcohol use may slightly elevate the risk of lung cancer, particularly in smokers. Quitting smoking is the best way to reduce lung cancer risk.
What investigations are done to diagnose lung cancer?
To diagnose lung cancer, doctors typically start with imaging tests such as chest X-rays and CT scans to look for any abnormalities in the lungs. If a suspicious area is found, a biopsy may be performed. This can be done through various methods, including bronchoscopy (using a thin tube with a camera to take tissue samples from the lungs) or needle biopsy (using a needle to extract tissue from a suspicious area).
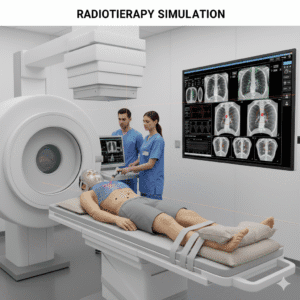
What are molecular tests, and why are they important?
Molecular tests analyze cancer cells for specific genetic mutations and biomarkers that can influence treatment decisions. For lung cancer, tests may check for mutations in genes like EGFR, ALK, and KRAS. Identifying these mutations helps determine whether targeted therapies or immunotherapies may be effective for a particular patient, allowing for more personalized treatment options.
What is targeted therapy, and how does it work?
Targeted therapy uses drugs that specifically target cancer cells with certain genetic mutations or characteristics while sparing normal cells. For example, medications like erlotinib (Tarceva) target EGFR mutations, while crizotinib (Xalkori) targets ALK rearrangements. This approach can lead to fewer side effects compared to traditional chemotherapy and is often used for advanced lung cancer with specific mutations.
What role does chemotherapy play in lung cancer treatment?
Chemotherapy involves using powerful drugs to kill rapidly dividing cancer cells. It is often used for lung cancer that is not amenable to surgery or when it has spread to other parts of the body. Chemotherapy may be given before surgery (neoadjuvant chemotherapy) to shrink tumors or after surgery (adjuvant chemotherapy) to eliminate any remaining cancer cells. Side effects can include nausea, fatigue, hair loss, and increased risk of infections.
How does immunotherapy work for lung cancer?
Immunotherapy helps the body’s immune system recognize and fight cancer cells more effectively. For lung cancer, drugs called immune checkpoint inhibitors (like pembrolizumab and nivolumab) block proteins that cancer cells use to evade immune detection. By inhibiting these proteins, immunotherapy can boost the immune response against the tumor, leading to better outcomes for some patients, particularly those with advanced disease.
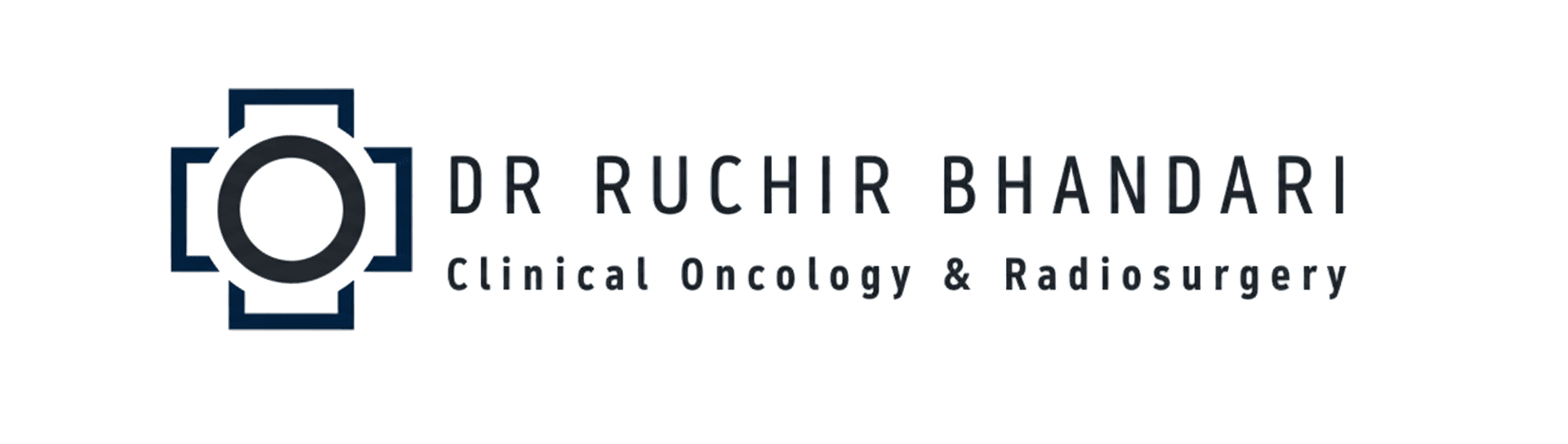
What is the role of radiotherapy in treating lung cancer?
Radiotherapy uses high-energy rays to kill cancer cells and shrink tumors. It can be used as a primary treatment for early-stage lung cancer, especially when surgery isn’t possible, or after surgery to eliminate remaining cancer cells. It’s also helpful for treating symptoms in advanced lung cancer, such as pain or obstruction. Side effects may include fatigue and skin irritation in the treatment area.
Will I need surgery for lung cancer?
Surgery is often an option for early-stage lung cancer. The type of surgery performed depends on the size and location of the tumor. Procedures may include lobectomy (removing a lobe of the lung), wedge resection (removing a small section of lung), or pneumonectomy (removing an entire lung). The decision for surgery considers factors like the patient’s overall health and lung function, as well as cancer characteristics.
What can I expect during follow-up appointments?
Follow-up appointments are crucial for monitoring recovery and detecting any signs of recurrence. These visits typically involve physical examinations, discussions about any new symptoms, and imaging tests like chest X-rays or CT scans. The frequency of follow-ups usually decreases over time but may remain regular for several years after treatment.
Are there genetic factors involved in lung cancer?
Yes, genetics can influence lung cancer risk. Certain inherited genetic mutations may increase susceptibility, particularly in individuals with a family history of lung cancer. Genetic testing can identify specific mutations, which may guide treatment options and help assess risk for family members. Consulting with a genetic counselor can provide valuable insights into personal and familial risk factors.
How important is exercise during treatment and recovery?
Exercise is beneficial for lung cancer patients both during and after treatment. Engaging in physical activity can help combat fatigue, improve mood, and enhance overall well-being. Tailored exercise programs, such as walking or pulmonary rehabilitation, are often recommended to support recovery and maintain lung function. It’s essential to discuss any exercise plans with your healthcare team to ensure they are safe and appropriate.
What rehabilitation services are available?
Rehabilitation services can significantly aid recovery after lung cancer treatment. Pulmonary rehabilitation is a specialized program that combines education, exercise, and support to help patients improve lung function and overall health. Other services may include physical therapy, occupational therapy, and counseling for emotional support. These programs are designed to help patients regain strength, manage symptoms, and improve quality of life.
What role does nutrition play during treatment?
Nutrition is a vital aspect of supporting health during lung cancer treatment. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help strengthen the immune system and maintain energy levels. Staying hydrated is also important, especially if experiencing side effects like nausea or loss of appetite. Consulting with a nutritionist can help tailor dietary recommendations to individual needs and preferences, ensuring that patients receive adequate nutrition throughout their treatment journey.