Immobilisation in Radiotherapy
Q1: What are immobilization methods in radiotherapy?
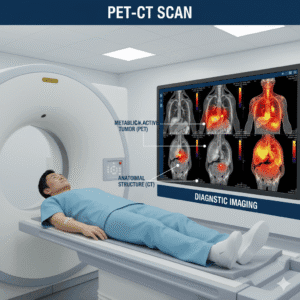
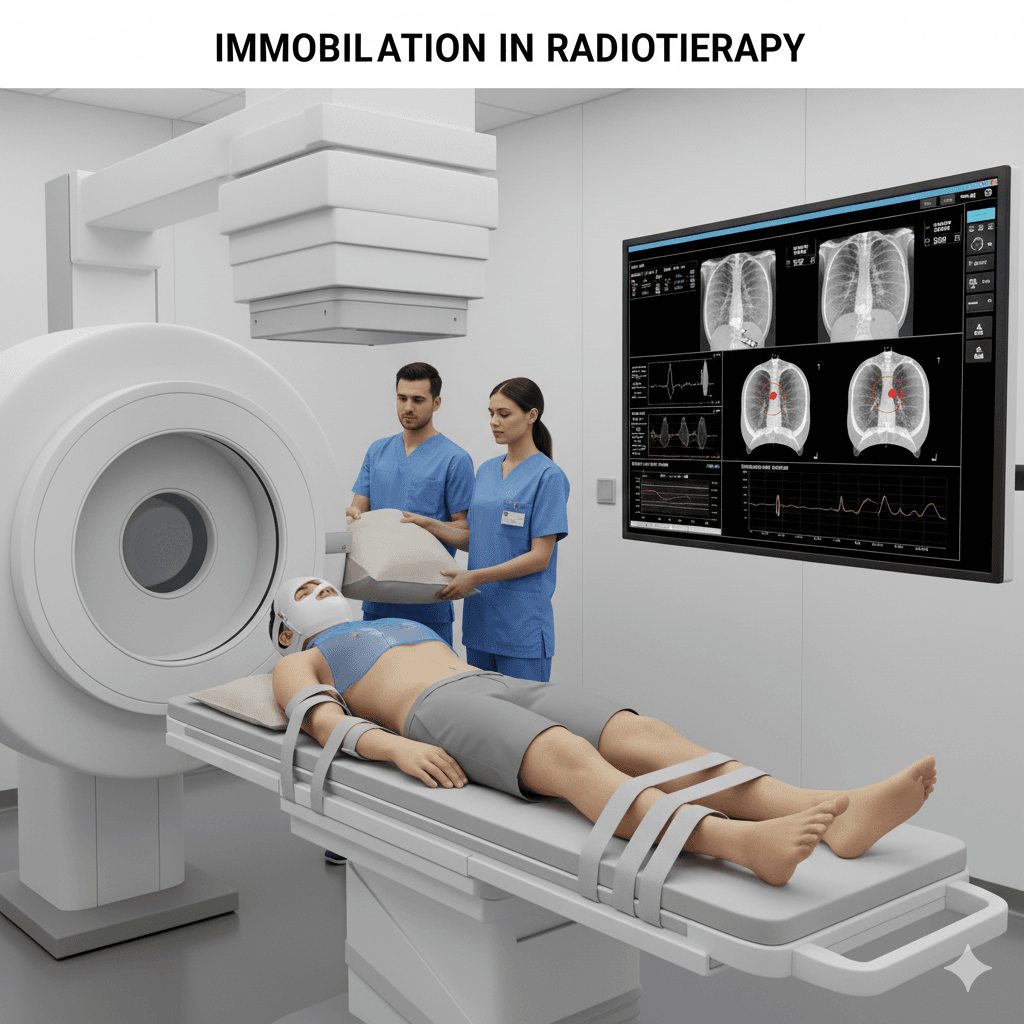
A: Immobilization methods in radiotherapy are techniques and devices used to keep a patient in a consistent, stable position during treatment. These methods ensure that the radiation is precisely targeted at the tumor, minimizing exposure to surrounding healthy tissues. Immobilization is crucial for the accuracy and effectiveness of radiotherapy, especially when treating areas like the head, neck, chest, or abdomen.
Q2: Why is immobilization important in radiotherapy?
A: Immobilization is important because:
- Precision: It helps maintain the same position during each treatment session, ensuring that the radiation is accurately delivered to the tumor.
- Consistency: By preventing movement, immobilization reduces the risk of targeting errors, which could lead to either under-treatment of the cancer or unnecessary radiation to healthy tissues.
- Safety: Proper immobilization minimizes the chance of side effects by keeping radiation focused on the intended area.
Q3: What are some common immobilization methods used in radiotherapy?
A: Common immobilization methods include:
- Thermoplastic masks: Custom-made masks are molded to the patient’s face and head, used to keep the head and neck still during treatment. These masks are commonly used for brain tumors, head and neck cancers, and other treatments involving the upper body.
- Body molds (vacuum cushions): A vacuum cushion is molded to the patient’s body shape, helping to hold the body in place during treatment. This method is often used for treatments involving the chest, abdomen, or pelvis.
- Bite blocks and mouthpieces: Devices placed in the mouth to stabilize the head and jaw during head and neck radiotherapy.
- Breast boards: Used for patients receiving breast cancer treatment, these boards help position and stabilize the upper body.
- Wing boards: These are used to support the arms in an elevated position during treatment, particularly for lung or breast cancer.
Q4: How are immobilization devices customized for each patient?
A: Immobilization devices are often custom-made to fit each patient’s unique anatomy:
- Assessment: The radiation therapy team assesses the area to be treated and determines the best immobilization method.
- Creation: For devices like thermoplastic masks or vacuum cushions, the patient will be positioned as they would be during treatment. The material is then molded to the patient’s body or face.
- Fitting: The patient tries on the device to ensure it fits comfortably and effectively holds them in the correct position.
- Adjustments: Any necessary adjustments are made to ensure the device is secure and the patient can maintain the position throughout the treatment.
Q5: What should I expect during the immobilization process?
A: During the immobilization process:
- Comfort: While the devices may feel snug, they should not cause pain or significant discomfort. The goal is to keep you still while ensuring you are comfortable enough to maintain the position during treatment.
- Positioning: You will be guided into the correct position, and the immobilization device will be applied. The radiation therapists will make sure you are stable and the device is properly aligned.
- Duration: Creating and fitting an immobilization device typically takes 15 to 30 minutes. During treatment sessions, you may need to stay in position for 15 to 45 minutes, depending on the complexity of the treatment.
- Communication: You will be able to communicate with your radiation therapists during the setup and treatment to ensure your comfort and address any concerns.
Q6: Are there any side effects or discomfort associated with immobilization?
A: Immobilization methods are generally safe and designed for comfort, but there can be some mild discomfort, such as:
- Pressure points: Some patients may feel pressure from the device, particularly if it fits snugly around the face or body.
- Claustrophobia: Some patients may feel anxious or claustrophobic when using a face mask or other close-fitting device. The radiation team can offer support and techniques to help manage these feelings.
- Minor skin irritation: Prolonged contact with the device may cause mild skin irritation, but this is usually temporary.
Your healthcare team will work with you to ensure that the immobilization device is as comfortable as possible and will make adjustments if needed.
Q7: How do immobilization methods improve the effectiveness of radiotherapy?
A: Immobilization methods improve the effectiveness of radiotherapy by:
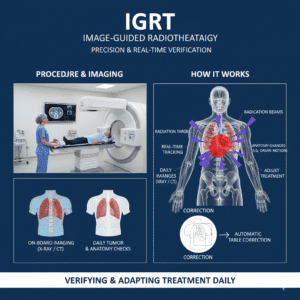
- Enhancing precision: By keeping the patient in a consistent position, immobilization ensures that radiation is precisely targeted at the tumor, maximizing the dose delivered to cancer cells while sparing healthy tissue.
- Reducing variability: Immobilization minimizes variations in patient positioning from session to session, leading to more consistent and effective treatment.
- Supporting advanced techniques: Many advanced radiotherapy techniques, such as intensity-modulated radiation therapy (IMRT) or stereotactic body radiotherapy (SBRT), require a high level of precision that is only possible with effective immobilization.
Q8: How do I know if immobilization will be part of my radiotherapy treatment?
A: Immobilization is typically part of radiotherapy treatment for cancers in areas that require precise targeting, such as the brain, head, neck, lungs, breast, and abdomen. Your radiation oncologist will determine the best immobilization method for you based on the location and type of your cancer, as well as the specific treatment plan.
If you have more questions about immobilization methods in radiotherapy or are concerned about the process, talk to your Radiation Oncologist to help you understand how immobilization will be used to improve the accuracy and safety of your treatment.
Related Post

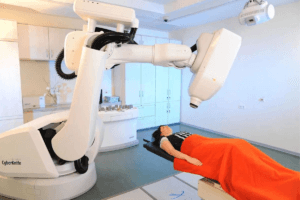
CyberKnife
August 6, 2024

Immunotherapy
August 7, 2024

MRI Linac
August 7, 2024
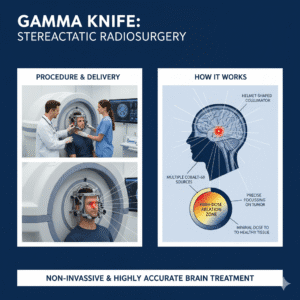
Gamma Knife
August 7, 2024
Cancer Screening
August 22, 2024
Gallery
Click below to book a clinic appointment
Ask More Questions Send Query On Email