Immuno-Histochemistry
Q1: What are IHC markers in cancer histopathology?
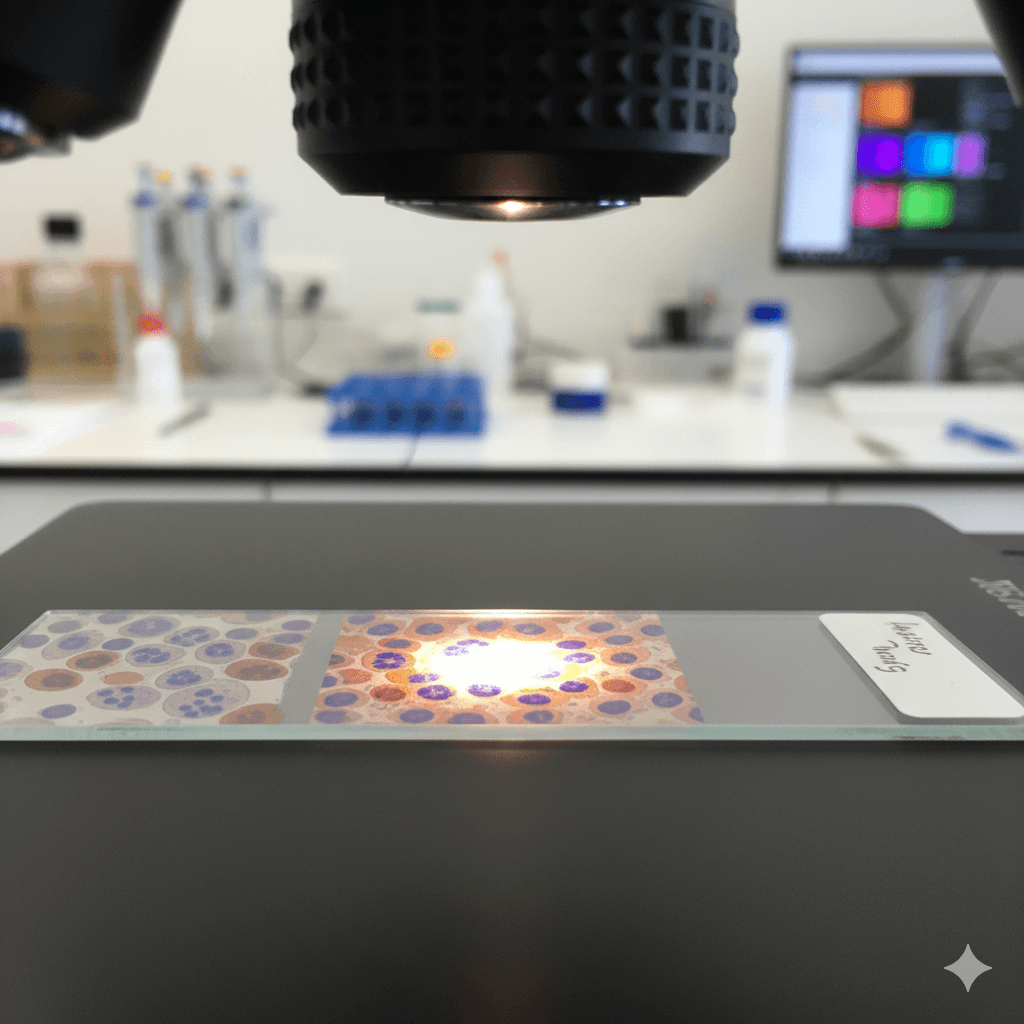
Immunohistochemistry (IHC) markers are specific proteins that can be detected in tissue samples using special staining techniques. In cancer histopathology, IHC markers help pathologists identify the type of cancer, its origin, and its characteristics by revealing the presence or absence of certain proteins in the cancer cells. These markers are crucial for diagnosing cancer, determining its aggressiveness, and guiding treatment decisions.
Q2: How does Immunohistochemistry (IHC) work?
IHC works by using antibodies that specifically bind to certain proteins (antigens) in the tissue sample. The antibodies are linked to a dye or a fluorescent marker, which makes the proteins visible under a microscope. When a tissue sample is treated with these antibodies, the presence of specific proteins can be seen as colored or fluorescent areas on the slide. This helps pathologists identify the type of cancer and understand its behavior.
Q3: Why are IHC markers important in cancer diagnosis and treatment?
IHC markers are important because they:
- Aid in diagnosis: IHC markers help confirm the type of cancer by identifying specific proteins that are characteristic of certain cancer types.
- Determine cancer origin: For cancers of unknown primary origin, IHC can help pinpoint the tissue or organ where the cancer started.
- Assess tumor characteristics: IHC markers can indicate how aggressive a tumor is and whether it is likely to respond to certain treatments.
- Guide treatment decisions: Some IHC markers are used to determine if a patient is a candidate for targeted therapies or immunotherapies.
Q4: What are some common IHC markers used in cancer histopathology?
Some common IHC markers include:
- HER2: Used in breast cancer to determine eligibility for targeted therapy with drugs like trastuzumab.
- ER and PR (Estrogen and Progesterone Receptors): Also used in breast cancer to assess hormone receptor status, which influences treatment options.
- Ki-67: A marker of cell proliferation, indicating how quickly cancer cells are growing.
- p53: A tumor suppressor protein that can indicate mutations in the gene associated with various cancers.
- PD-L1: Used to evaluate eligibility for immunotherapy, particularly in lung cancer and melanoma.
- CD markers (e.g., CD20, CD3): Used to classify lymphomas and leukemias by identifying specific types of immune cells involved.
Q5: How are IHC markers used to guide cancer treatment?
IHC markers guide cancer treatment by providing information about the tumor’s biology:
- Targeted therapy: For example, HER2-positive breast cancers can be treated with HER2-targeted drugs, while ER-positive breast cancers may respond to hormone therapy.
- Immunotherapy: Tumors that express high levels of PD-L1 may be more responsive to immune checkpoint inhibitors, a type of immunotherapy.
- Prognosis: Markers like Ki-67 can give insights into how aggressive the cancer is, helping doctors tailor the treatment plan accordingly.
Q6: How is a tissue sample prepared for IHC testing?
The preparation of a tissue sample for IHC testing involves several steps:
- Tissue collection: A sample of the tumor is obtained through a biopsy or surgery.
- Fixation: The tissue is preserved in a fixative (usually formalin) to prevent degradation.
- Embedding: The tissue is embedded in a block of paraffin wax to allow for thin slicing.
- Sectioning: Thin slices of the tissue are cut and placed on microscope slides.
- Staining: The slides are treated with antibodies that bind to specific proteins, followed by a detection system that makes these proteins visible.
Q7: Are there any limitations to IHC testing?
While IHC is a powerful tool, it does have some limitations:
- False positives/negatives: The accuracy of IHC depends on the quality of the antibodies used and the sample itself. In some cases, nonspecific staining or poor-quality samples can lead to inaccurate results.
- Limited scope: IHC can identify the presence of specific proteins, but it cannot provide detailed information about the genetic mutations underlying cancer.
- Requires expertise: Accurate interpretation of IHC results requires a skilled pathologist who can distinguish between meaningful staining and background noise.
Q8: How do IHC results affect a patient’s treatment plan?
IHC results play a critical role in shaping a patient’s treatment plan by providing detailed information about the cancer’s type, grade, and molecular characteristics. For instance, if a breast cancer tumor is found to be HER2-positive and ER/PR-negative, the treatment plan may include HER2-targeted therapy rather than hormone therapy. The information from IHC tests helps oncologists choose the most effective treatment options, improving the chances of successful outcomes.
If you have more questions about Immunohistochemistry (IHC) markers or how they are used in cancer diagnosis and treatment, talk to your Oncologist to know how IHC results will influence your specific treatment plan and what to expect from the testing process.
Related Post

CyberKnife
August 6, 2024

Immunotherapy
August 7, 2024

MRI Linac
August 7, 2024
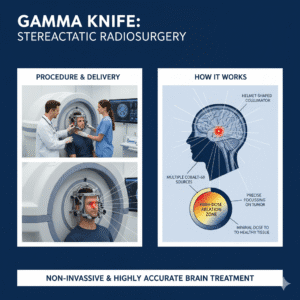
Gamma Knife
August 7, 2024
Cancer Screening
August 22, 2024
Gallery
Click below to book a clinic appointment
Ask More Questions Send Query On Email